Unveiling the relationship between immune system and infectious diseases
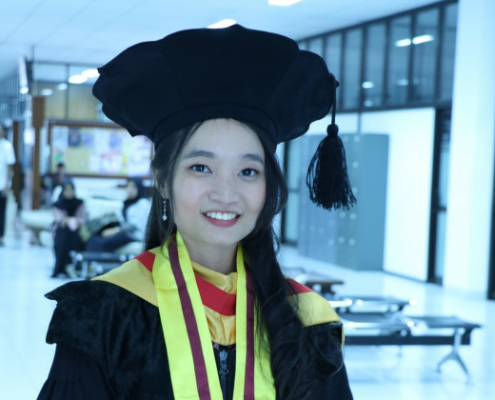
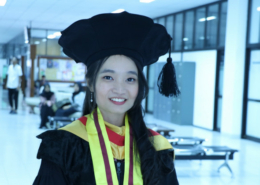
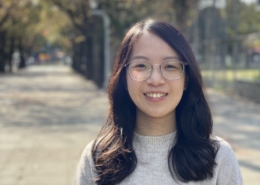
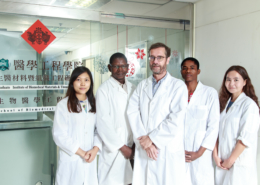
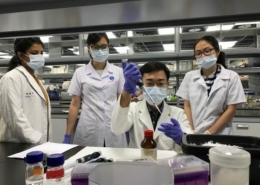
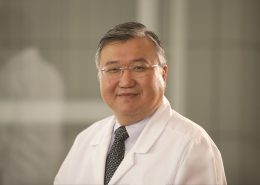
Assistant Professor Laurensia Denise Utami Putri of TMU Graduate Institute of Clinical Medicine Shares Groundbreaking Research on the Immune System
Source: College of Medicine
Published on 2023-11-06
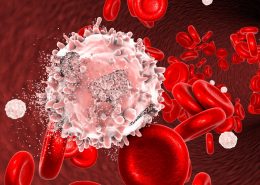
The immune system has long been studied for its role in protecting the human body from disease development.
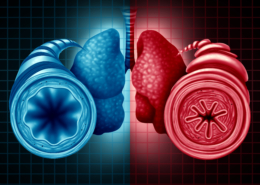
Physical barriers such as skin and mucosal membranes serve as the first protector so that we don’t get ill every other day, even though many infectious bacteria and viruses frequently come into contact with us. Immune cells and antibodies further orchestrate a series of responses to eliminate pathogens that gain the entry into our body while also preventing harm to ‘self’ tissue. In brief, the “innate” immunity responded rapidly to any pathogen encounter, and the later “adaptive” immunity performed specific and targeted elimination of the pathogen.
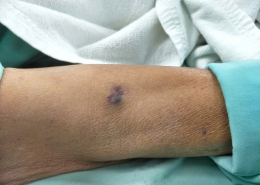
Graduating as a Medical Doctor from Indonesia, a country with a tropical climate, I commonly found patients with infectious diseases presenting with distinct signs and symptoms, some being critically ill while some barely reporting any. It is when I learned that the immune system plays a vital role not only in pathogenesis but also in disease progression and response to treatment, thus driving my interest to study further about immunology.
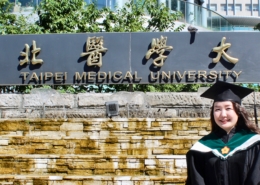
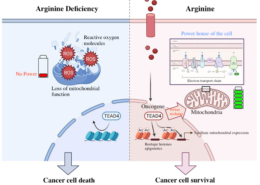
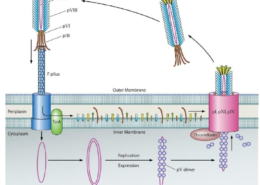
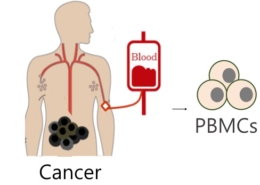
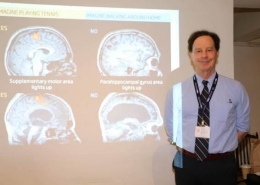
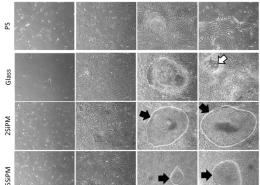
I did my Ph.D. at Taipei Medical University, where I got acquainted with proteomics assay, an advanced and powerful method to dissect the protein landscape from a single cell. Adapting proteomics, we studied the response of macrophage, one of the innate immunity’s mercenaries, to heat-killed Mycobacterium tuberculosis stimulation, and proposed a molecular mechanism for its activation in a lung cancer setting. Proteomics can also serve as an approach to studying the expression and activity of multiple immune cells simultaneously. We reported immune cell signatures which include T cells, B cells, monocytes, and NK cells, in lung cancer patients receiving chemotherapy which may predict progression-free survival.
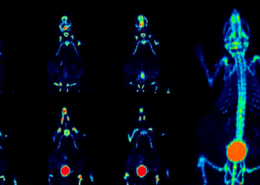
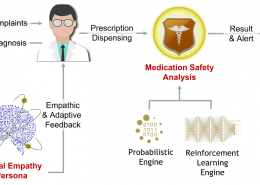
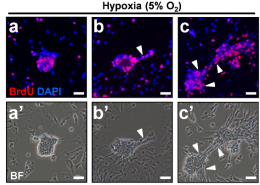
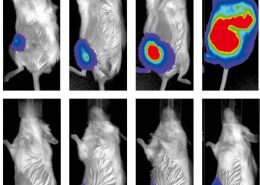
With the nature of communicable diseases, COVID-19 came to global attention with its widespread transmission. Other than the novel pathogen, studies are directed at unraveling the host’s immune responses, which lead to the discovery of preventive vaccines and therapeutic approaches. Our team previously mapped an immune cell landscape mimicking those with a severe infection in COVID-19 patients presented with long viral positivity (up to 76 days) although they showed mild symptoms throughout the course of the disease. Adapting multi-panel flow cytometry assay, we also discovered distinct B and NKT cell responses in end-stage renal disease patients with delayed response to COVID-19 vaccination. We also recently discovered attenuated inflammatory cytokine secretion along with low T cell number in recovered patients, which should raise cautiousness to the possibility of occult immune dysregulation and exhaustion following COVID-19 infection.
I plan to continuously engage in studies that are close to the clinical needs, especially those related to pulmonary diseases including COVID-19, Tuberculosis, and lung cancer. I would be interested in conducting more translational research which could produce meaningful and applicable results, translating basic science discoveries more quickly and efficiently into practice.





















-260x185.jpg)












































與連江縣衛生福利局陳美金局長簽署醫療合作備忘錄-260x185.jpg)
















期許永續發展成為醫療產業新契機。-260x185.jpg)











































































































































































































































































































































































































與連江縣衛生福利局陳美金局長簽署醫療合作備忘錄-80x80.jpg)